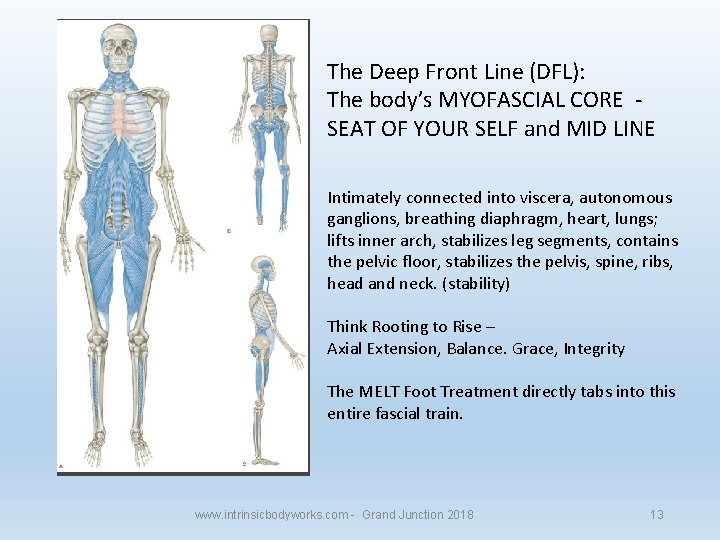
The Deep Front Line (DFL, from Thomas Meyers Anatomy Trains) is one of our most fundamental tracks of soft tissue. It is the soft tissue equivalent and partner of our skeleton (especially the axial) and is what most fundamentally holds the core of our structure together when it comes to musculature and soft tissue. To explain its role to my patients I tell them to think of a bridge. The concrete or steel of the bridge is your skeleton/spine (primarily axial) while the tissues of the deep front line are like the tension cables. Together their compression and tension hold together as the foundation of our structure with excellent integrity, if everything is doing its job. As long as there is no break or other structural problem with the skeleton (that concrete/steel part of the bridge) then we don’t have to worry about that. The majority of the problem comes in when there is problems in regulating tension in the soft tissues of the deep front line. All of you reading this know it’s not a matter of isolated or simple chronic tightness or ‘over use’ that causes tension disparities, nor is it because the muscles are ‘weak’ so we won’t even cover that aspect here (it seems half my articles are just explaining the premise of neuromuscular control theory).
The deep front arm line is one that is overused, tight, and of course weak on basically everyone from one degree or another. Each bundle of fascia is connected to another bundle of fascia, which means that everything in the body is connected to everything else. The 12 lines are: Superficial Front LineRuns from the top of the toes up the front of the leg and up the torso to the top of the sternum, and passes along the side of the neck to the back of the skull.

So what problems do happen with the DFL tension? Simply stated one length of the deep front line either gets too tight or too loose for the overall DFL to hold the tension it needs for dynamic structural integrity. When one length tightens too much…another has to slacken. When one slackens, another has to tighten. Any of you who do neuromuscular work and are familiar with anatomy trains can probably without hesitation tell me what 75% of someone’s deep front is up to (facilitation or inhibition) without even looking; and you probably have some notion for what’s causing what. This is because while individual circumstances and variables will change exactly what’s going on, the overall approach that the MCC takes to keep the structure safe is generally the same: compress and limit range of motion (there are some joints and injuries where this is not the case, such as ankle injuries). Anything that can compress is usually used for this function, and anything that will decompress is usually at least down-regulated if not inhibited.
The overall effect commonly looks like an undulation of facilitated, inhibited, facilitated, inhibited, etc. though not always. For example I most typically find the toe flexors and or post tib working for most if not all of the adductors. The pelvic floor is either facilitated for itself (commonly posterior to anterior but it can be all or nothing as well, especially after pregnancy/genital surgeries; episiotomies are common culprits) or for part of the core above. The iliacus is commonly facilitated for the psoas, though honestly I don’t tend to consider the psoas and iliacus as part of the deep line structure in this way, but I’ll leave that opinion for another article. The TVA, RA and multifidus is typically inhibited, with the TVA having the hardest job working (95% of the time or more it doesn’t; if you find one functioning, DON’T BELIEVE IT. Mess with things until it fails. If they’re on your table with a complaint, I don’t believe their TVA. An eccentrically loaded diaphragm is probably making it look like a pass.) followed by the RA and then the multifidi closely behind. The pelvic floor may be working for one of the aforementioned 3 primary core muscles, though the next step in the chain is the diaphragm which because it is attached to a balloon it’s an amazing central hub of facilitation. Commonly it will hold tension, even if only eccentrically (check my article on eccentric contractions causing false positives) to give the MCC enough sense of tension to allow things to function, including the TVA.
The deep front line continues up along the spine and throughout the thoracic cage including wrapping around the lungs and other organs. If your patient has pleurisy, see if clearing the deep front line helps as the condition is generally considered idiopathic but my money is on some form of severe deep front line dysfunction. As we go proximal we get into the deep neck flexors, which are commonly inhibited by a whole mess of things (extensors, especially suboccipitals, 1-2 of the scalenes, and or a levator), then into the floor of the mouth, the tongue, the masseter, and the temporalis. Unsurprisingly, this last group of structures tend to be highly facilitated. With the jaws wide range of motion and extreme strength, let alone common use, it is a shoe in for holding tension at the top of the chain so is very typically facilitated for large stretches of the core in the DFL as well as the neck, causing TMJ ‘syndrome’ frequently (even if they aren’t aware, see how evenly their jaw opens at the TMJ) and occasionally with attached tinnitus, let alone tension headaches around the temporalis.
 So to recap and add a bit: we often see the deep posterior calve compartment working for the adductors, as well as the psoas, sometimes more (I’ve seen iliacus, TVA, RA, etc.). The pelvic floor, diaphragm and jaw commonly are facilitated for any of the three main core muscles; the TVA, RA, and multifidi/erectors (sometimes one to one, sometimes one to all). The neck flexors can be do the jaw or something else in the deep front line but usually I find that a local relationship to the neck/cervical vertebrae as part of a cervical compression strategy (more in my article on c2 displacement concerning cervical/axial compression strategies).
So to recap and add a bit: we often see the deep posterior calve compartment working for the adductors, as well as the psoas, sometimes more (I’ve seen iliacus, TVA, RA, etc.). The pelvic floor, diaphragm and jaw commonly are facilitated for any of the three main core muscles; the TVA, RA, and multifidi/erectors (sometimes one to one, sometimes one to all). The neck flexors can be do the jaw or something else in the deep front line but usually I find that a local relationship to the neck/cervical vertebrae as part of a cervical compression strategy (more in my article on c2 displacement concerning cervical/axial compression strategies).The thing to remember is that this is not a facilitation/inhibition relationship of ACTION, but one of tension. While one adductor may inhibit another via reciprocal inhibition as a functional antagonist, and a gastroc head may cause plantar flexon when there is no extension of the hip for ambulation, this set of relationships is most purely one of creating adequate structural tension around a strategy of compression. This means that while the pelvic floor, diaphragm and TMJ musculature are facilitated, releasing them does not necessarily fix the problem. Typically these structures tighten because something else fails and tension is required. As I tell my patients; if you take a week off sick and come back to find your co-worker has been doing your job, is that their fault? The work needed to be done, so they did it, don’t blame them. But if you can’t get your work done because of a mugger? Yeah, that’s the guy to take care of.
As always I urge people to find the actual culprit; releasing a facilitated diaphragm is no better than our previous paradigm of stretching a muscle because it’s tight. You must ask and find out why! I do not release these muscles very frequently because they are victims being forced to work too hard in most instances. Sometimes a local trauma will change the situation but most of the time it is simply a global stability strategy and you need to find the source. I may treat some symptomatically (but never the diaphragm) at these levels, but you aren’t treating the source unless you have reason to know it’s the source.
This brings us to finding the original cause, which generally goes out of the scope of this article but we’ll give you a direction. 90%+ of what I treat is scars, concussions, broken bones and joint injuries, or they are being referred out to deal with limbic trauma (see my article on limbic/MCC function and their interplay in rehab work). There are of course other injuries, but these cover the main sources of ‘original causes’ which are driving the body to create a global compensation strategy in the first place, which again is marked by axial compression and is likely the cause of your deep front line dysfunction.
So let’s take an example: Patient A presents with chronic headaches, neck tightness, and low back pain. Upon initial testing you find the flexor hallucis longus working for the majority of the adductors and the psoas, the masseter working for the neck flexors and diaphragm working for the TVA. A pretty typical pattern, but when we get into the history we find that this patient had a vaginal tear (or episiotomy) during birthing and that she has also had urine urgency and poor sense of bladder fullness (when she has to go, she has to go immediately, and probably leaks very easily) as well as frequent constipation. This kind of injury is a severe insult to the deep front line and given its location on not just the deep front line, but the anterior core and on the genitals themselves the body frequently feels highly unstable and reacts globally.
Following the likely chain of compensations from her history and symptoms, we can see that her anterior pelvic floor is inhibited (she also reports not being able to feel a kegel, or if she does she can tell it is very weak and minimal; she may even feel pain during sex which may also be from a facilitated pelvic floor) and while it may be from another cause (non-neuromuscular) her posterior pelvic floor is likely to be facilitated for it to hold appropriate distal tension. By doing spot releases or an anti-kegel followed by a kegel you may or may not see improvements in neural connection to the anterior pelvic floor, but this isn’t the cause anyway so I am not concerned.
Moving on and up this instability leads to axial compression, likely including one hip, SI joint and an elevated shoulder on the same side (typically the side that is most unstable) which is capped (again commonly but not always) with an inhibited levator, resulting either in defensive tightness pulling the C2 and other vertebrae out of place or the other levator/scalenes which are facilitated are responsible for the subluxation. The C2 deviation or the SI jam ‘directly’ inhibit the TVA and cause even more dysfunction. A non-functioning TVA, faciliatory diaphragm, and cervical compressing secondary respirators all throw out the breathing patterns and seal the global compensation pattern.
 The increased tension on the TMJ musculature and the compressing elements of the neck cause a lot of global tension to be routed through them, resulting in neck tightness and chronic headaches. A jammed SI and non-functioning TVA would be enough by itself to cause low back pain, but in all reality we would also have no psoas function and probably only one capable QL.
The increased tension on the TMJ musculature and the compressing elements of the neck cause a lot of global tension to be routed through them, resulting in neck tightness and chronic headaches. A jammed SI and non-functioning TVA would be enough by itself to cause low back pain, but in all reality we would also have no psoas function and probably only one capable QL.Going back to the likely original cause in this case, we instruct the patient to assist us in testing the pelvic floor scar and then releasing it. If this is the original cause we expect it to be, the SI should no longer be very causally involved, giving us a big jump in hip and lumbar spine stabilizer function (TVA, psoas, QL) and release the structurally mandated tension on the TMJ musculature. The pelvic floor itself may or may not immediately respond but I generally find unless there is a more severe injury at play, the patient should be able to feel a difference in her kegel (but again, not always right away!).
She may need symptomatic approaches for a time in addition, so other than the fundamental homework that would be scar release to kegels (yes, we on rare occasions assign kegels!), releasing the SI jam to a severely inhibited TVA via dying bug and release of one levator to another or suboccipitals to the deep neck flexors would be an appropriate approach to treatment.

Another worthy mention is that if someone has symptoms such as these; especially something like TMJ, there may be nothing you can do to permanently resolve it if they are a persistent gym chewer. Loading up extra pressure on the masseter will strongly reinforce the compensation despite your best homework releases in many cases, and part of the thing to realize is that it isn’t just additional time chewing. Because of the thickly ‘chewey’ nature of gum we tend to try to “smash the shit out of it,” as I put it to my patients (they laugh and then realize it’s really quite true). They really need to ditch the gum or their neck/head/jaw issues are likely there to stay forever.
Similarly, breathing patterns MUST be addressed to get the core (especially the TVA) working again and the diaphragm/secondary respirators regulated. Simple diaphragmatic breathing (having them hold their hands on, but don’t push, right below the belly button while supine and practice pushing their hands out with their low stomach during their inhale; starting and contributing the vast majority of their breathing volume with their abdomen, only having chest involvement near the end.
So there is a general approach and info to the role of the deep front line; the soft tissue foundation of our structure (just for more examples; the supporting rope for a mast, or the lines for a tent). Normalizing someone’s deep front line is one of the most profound things you can do for them and if you successfully clear it (not that you won’t have to venture out of the deep front line at times to treat it) their symptoms won’t likely stay gone for long. The next step would be making sure their rotational lines work as all real human movement is a mixture of rotation and counter rotation; when these don’t work properly then force must be transferred into other planes and inappropriate structures causing wear and a load of issues, but that’s for another day.
Filed under: The Practitioners Corner
Like this post?Subscribe to my RSS feed and get loads more!
Fascia. A term that just a few years ago had little meaning in the performance and fitness industry. The days of foam rollers collecting dust in the corner have been replaced with courses specializing in fascial dissection, trigger point release and rehab programming related to fascial lines.
As we enter this paradigm shift in the way we look at human movement, corrective exercise and performance I have seen an increase in the appreciation for the foot & the ankle. With almost every fascial line passing through the bottom of the foot, professionals worldwide can appreciate how integrated the foot and the ankle really is with the rest of the body.
In this article series we are going to take the concept of foot function and fascia further than any course or textbook on the market. This first article is dedicated to taking a closer look at how the fascial lines influence great toe range of motion.
Let’s take the importance of fascia and foot function one step further and look at propulsion!
Propulsive Phase of Gait
Whether we are walking, running or jumping – push-off or propulsion is characterized by dorsiflexion of our digits at the metatarsophalangeal joint (MPJ). The joint that takes a majority of the forces during push-off and is responsible for the release of elastic energy is the 1st MPJ.
As much as dorsiflexion of the 1st MPJ may seem like a simple biomechanical movement, it is actually quite complex – requiring timed control and activation of our fascial slings.
What Is Deep Fascia In Muscles
Let’s take a closer look at the 1st MPJ.
The First Metatarsophalangeal Joint
The 1st MPJ is formed by the base of the proximal phalynx and the head of the 1st metatarsal. Sitting directly under the head of the 1st metatarsal and lying within the tendons of the flexor hallucis brevis are the sesamoids. Inserting on the medial aspect of the proximal phalynx is the abductor hallucis which is opposed laterally by the adductor hallucis.
As we begin to transition onto the forefoot and into propulsion, what dictates the range of motion of the 1st MPJ is first metatarsal position in the sagittal plane. The image below illustrates how an elevation of the first metatarsal in the sagittal plane can block the dorsiflexion or gliding the proximal phalynx over the head of the first metatarsal.
So what dictates the position of the first metatarsal in the sagittal plane thereby playing a role in 1st MPJ dorsiflexion at propulsion?
If you guess the Spiral Line you are correct!
The Spiral Line – Expanded Version
Youtube Deep Front Line Fascia
In Thomas Myers’ Anatomy Trains he describes the lower part of the Spiral Line as the tibialis anterior as it joins the peroneus longus at the level of the base of the 1st metatarsal.
Often referred by Myers at the “stirrup” of the foot, I want to expand upon this concept a little further and demonstrate how the Spiral Line plays a bigger role in propulsion than you may think!
The tibialis anterior muscle runs down the anterior aspect of the lower leg to insert on the medial aspect of the foot on the medial cuneiform (90%) and the base of the 1st metatarsal (10%). Joining plantarly is the peroneus longus tendon which runs along the lateral aspect of the lower leg, behind the lateral malleolus and under the cuboid to insert on the base of the 1st metatarsal (90%) and medial cuneiform (10%).
With 90% of it’s insertion on the base of the 1st metatarsal, the peroneus longus plays an important role in plantarflexion of the 1st metatarsal allowing dorsiflexion of the 1st MPJ during propulsion.
So does this mean that for optimal propulsion and dorsiflexion of the 1st MPJ all we need to do is ensure proper activation of the peroneus longus muscle or the Spiral Line?
Unfortunately it isn’t that easy! Proper activation of the Spiral Line is actually integrated with another fascial line – the Deep Frontal Line.
The Deep Front Line
For the Deep Front Line again we return to Myers Anatomy Trains.
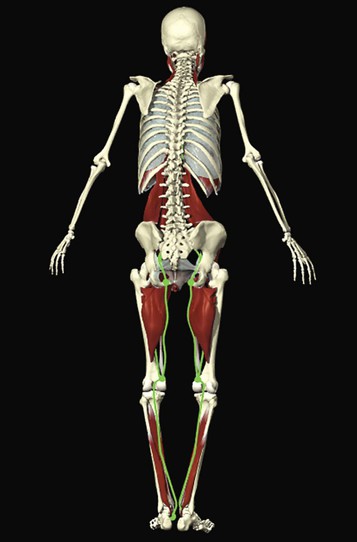
In the plantar foot the Deep Front Line consists of the deep posterior leg compartment including the posterior tibialis, flexor hallucis longus and flexor digitorum longus. For the purpose of this article we are going to focus soley on the posterior tibialis.
Running posterior to the medial malleolus and along the medial aspect of the foot, the Posterior Tibialis inserts onto the navicular. After attaching to the navicular the Posterior Tibialis fans out and has 9 osseous and fascial attachments which includes:
– every tarsal bone (except the talus)
Deep Front Line Fascia
– every metatarsal (except the 1st)
– peroneus longus tendon
– flexor hallucis brevis muscle
This fascial attachment between the posterior tibialis and the peroneus longus joins the Deep Front Line to the Spiral Line allowing for more integrated foot biomechanics.
EMG studies have shown that the posterior tibiailis activates prior to the peroneus longs during the gait cycle which means this fascial integration between the PT and PL prepares the foot for propulsion.
With the posterior tibialis as a driver of subtalar joint supination or inversion just prior to heel lift, a reflexive activation of the Spiral Line leads to stabilization of the 1st metatarsal by the peroneus longs – allowing for dorsiflexion of the 1st MPJ and propulsion.
Client & Athlete Application
When assessing optimal propulsion in our clients and athletes remember the function of the Spiral Line and Deep Front Line on 1st MPJ dorsiflexion. A limitation in 1st MPJ dorsiflexion or power at propulsion may be related to an impairment in posterior tibialis strength.
To optimize posterior tibialis strength in clients and athletes integrate barefoot exercises such as short foot which picks up the navicular bone and stimulates the Deep Front Line. In addition single leg exercises can used the strength the posterior tibialis and it’s co-activation patterns with the gluteus medius and maximus.
Take a look at our webinar for related information: Optimizing Power at Push Off | High Gear vs Low Gear Position with Dr Emily Splichal
To learn more about about foot function and barefoot strengthening please visit:
Deep Front Arm Line Fascia
Are you barefoot strong?